Uncovering Disparities in COVID-19 Hospital Treatment
How did gaps in treatment during the COVID-19 pandemic contribute to prolonged hospital stays, septic shock, and increased mortality? FLCCC Co-founders examine research from the 2024 CHEST conference.
Full Video
Speakers: Dr. Jose Iglesias, Dr. Paul Marik, Dr. Joseph Varon
This week, join FLCCC co-founders Dr. Joseph Varon and Dr. Paul Marik, along with FLCCC Senior Fellow and co-founder Dr. Jose Iglesias, for an in-depth discussion on findings presented at the CHEST conference. Drawing insights from a 50-state survey of U.S. adults, the panel will examine trust in physicians and hospitals during the pandemic and reveal how discrepancies in care affected hospitalized COVID-19 patients.
“There are a fair number of disparities between racial and ethnic groups for a variety of reasons.” – Dr. Jose Iglesias
It’s almost hard to recall a time before the COVID-19 pandemic reshaped the landscape of healthcare. Yet one fact remains unchanged: disparities in health outcomes among racial and ethnic groups have long been entrenched in our healthcare system. These inequities, though largely overlooked, have silently influenced lives for decades, only to be thrust into the spotlight by the pandemic.
Rooted in unequal access to care, systemic socioeconomic barriers, and a legacy of mistrust in medical institutions, these disparities converged with the pandemic’s challenges. As Dr. Jose Iglesias observes, the data paints a stark picture: COVID-19 mortality rates, hospital stays, and overall health outcomes disproportionately affected minority populations.
“There are significant racial disparities in COVID-19 morbidity,” Dr. Iglesias explained. In this webinar, alongside fellow FLCCC co-founders Dr. Paul Marik and Dr. Joseph Varon, Dr. Iglesias will share key findings that were initially presented at the CHEST Annual Meeting, a premier conference focused on advancements in pulmonology, critical care, and sleep medicine organized by the American College of Chest Physicians (ACCP).
Your Support Makes Webinars Possible Every Week
The FLCCC Weekly Webinar provides a platform for open dialogue, expert insights, and life-changing information—all thanks to your support. Together, we’re creating a space where truth and transparency in healthcare thrive.
Septic Shock Outcomes Predicted COVID-19 Inequities
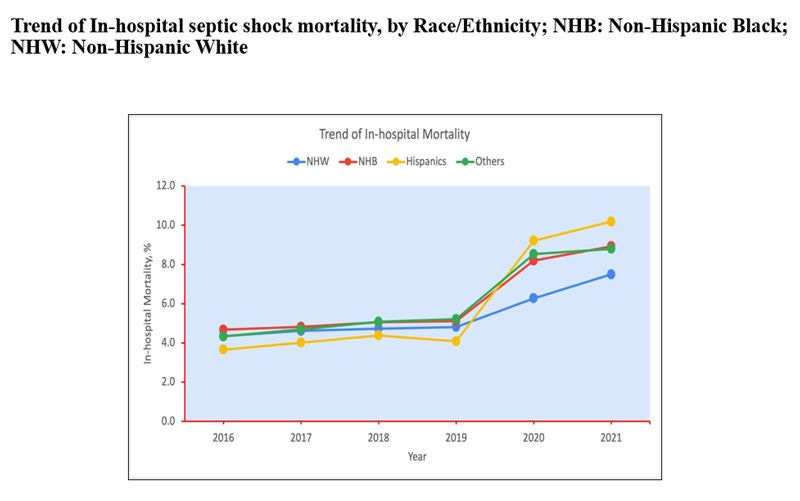
Before the pandemic, his team had been investigating disparities in septic shock outcomes among critically ill patients. This work became the foundation for understanding broader inequities during COVID-19.
“Septic shock was the initial clue,” Dr. Iglesias explained.
The rise in severe COVID-19 cases exposed these disparities on an unprecedented scale. Minority groups faced higher rates of severe illness and death, often stemming from vulnerabilities that developed long before hospitalization. “The drivers of these disparities,” Dr. Iglesias emphasized, “occur way before the patient gets critically ill and ends up in the ICU.”
Analyzing Mortality Rates by Race and Ethnicity
“The data showed clear disparities, even when accounting for socioeconomic and clinical factors.” – Dr. Iglesias
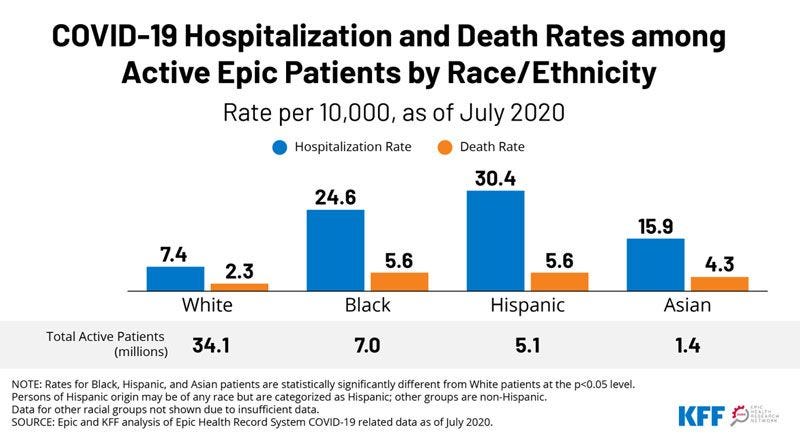
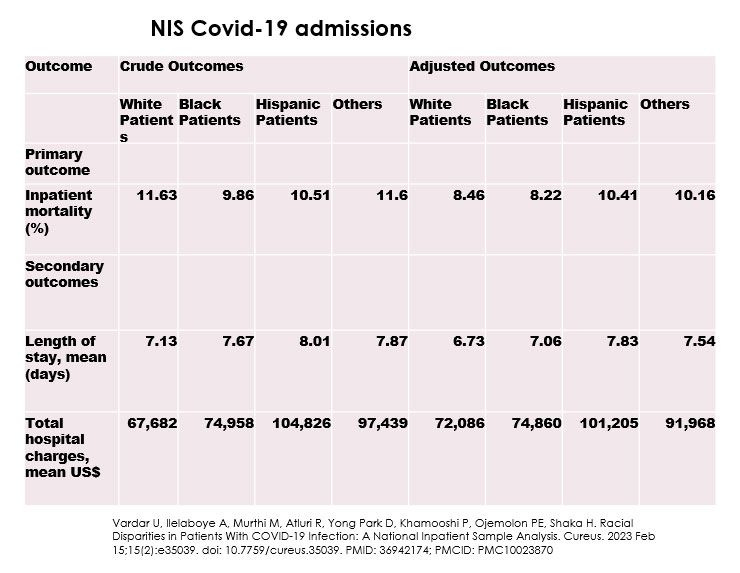
When Dr. Iglesias and his colleagues analyzed data from the National Inpatient Survey (NIS) and other sources, they found that Black, Hispanic, American Indian, and Alaska Native patients experienced disproportionately higher COVID-19 mortality rates compared to non-Hispanic White patients.
Even after adjusting for socioeconomic factors and pre-existing health conditions, non-White patients faced worse outcomes—a sobering reminder of how deep these inequities run. The findings pointed to systemic issues in healthcare delivery, resource allocation, and access to care, painting a stark picture of health inequity.
Declining Trust in the Healthcare System
“Historical events like Tuskegee have left a lasting scar on trust.” – Dr. Iglesias
One of the most insidious factors driving these disparities is a lack of trust in the healthcare system. For many, this mistrust is based in historical injustices, like the infamous Tuskegee syphilis study, where minority populations were exploited and deceived by medical authorities.
Dr. Iglesias noted that during the pandemic, trust in physicians and hospitals fell sharply, from 71% in April 2020 to just 40% by January 2024. This decline had real consequences: patients delayed seeking care and often arrived at hospitals only when severely ill.
Dr. Varon reflected, “By the time patients came to us, they literally had to be dying before they came to the hospital.” Undocumented patients, for example, avoided care out of fear—fear of financial ruin, deportation, or even mistreatment.
These patterns of avoidance only deepened the health inequities exposed by the pandemic.
The Role of Financial and Systemic Factors
“Financial incentives often overshadow patient care.” – Dr. Paul Marik
The pandemic also revealed troubling systemic issues within healthcare. As Dr. Marik noted, financial incentives often took precedence over patient welfare, resulting in profit-driven policies and protocols that failed to prioritize equity or health outcomes.
According to Dr. Igelsias, poor quality of care, influenced by racial and cultural biases, compounded these issues. Minority patients often reported inadequate communication, dismissive attitudes, and insufficient attention to their concerns. Combined with external factors like crowded living conditions, limited access to healthy foods, and systemic barriers to healthcare, these dynamics made a bad situation worse for many minority groups.
Building Toward Equity in Healthcare
“The driving factors influencing these outcomes likely develop long before patients are hospitalized.” – Dr. Iglesias
The pandemic has helped us to understand many of the once hidden cracks in our healthcare model. Medical care disparities represents yet one more crack to deal with. Achieving health equity requires addressing the root causes of disparities—early and comprehensively. Structural inequalities and deep-seated mistrust must be tackled head-on.
As Dr. Iglesias remarked, “It’s time to at least bring honest medicine back.” Rebuilding trust between patients and providers is critical. This means prioritizing transparency, fostering patient-physician relationships that bridge cultural divides, and ensuring that financial incentives do not compromise care quality.
“It’s been a long road,” said Dr. Marik as he reflected on his pandemic journey, fraught with challenges, but he emphasized the importance of using this experience to inform systemic change. From rethinking hospital protocols to addressing community-level vulnerabilities, the journey toward health equity is far from over.
Turning Lessons Into Action
The disparities laid bare by COVID-19 are not anomalies; they are symptoms of a broken system. Moving forward, healthcare must adopt a holistic approach—one that considers the socioeconomic and environmental factors shaping health risks, restores trust through honest communication, and implements policies to ensure equitable outcomes.
One important consideration: if healthcare was cheaper and more effective, wouldn’t that do a great deal to bridge the gap? If patients could get a cheap prescription for a repurposed medicine like ivermectin or hydroxychloroquine, perhaps they could stay out of the hospital all together.
If today’s webinar has provided valuable insights, we encourage you to support the FLCCC Alliance. Your contributions allow us to continue advancing critical research, sharing cutting-edge medical science, and advocating for equitable healthcare solutions. Whether you’re a healthcare professional, a patient advocate, or someone passionate about health equity, your support helps ensure that lifesaving knowledge reaches those who need it most.






No amnesty for DEPRAVED-HEART MASS MURDER (which was, in fact, premeditated)
ALL THE PROOF NEEDED FOR REAL COVID TREATMENT HAS BEEN DEMONSTRATED FROM EARLY 2020 WITH PANDEMIC TIMES "GOLD STANDARD EVIDENCE" – THE RESULTS FROM REAL DOCTORS WHO TREATED REAL COVID PATIENTS.
ALL THE PROOF NEEDED for 1) the early outpatient treatment for covid, for 2) the asap covid treatment in the ER (or doctors. office outpatient "ER") which either stabilizes the the covid patient and sends them home with prescriptions or begins proper treatment prior to hospital admission and for 3) the best in hospital covid treatment, - all using combinations of safe and effective, low cost, available drugs etc HAS BEEN DEMONSTRATED, from early in the pandemic, noised abroad to "people" in the cdc and niaid and all, and continually improved WITH THE PANDEMIC "GOLD STANDARD EVIDENCE" – THE RESULTS FROM REAL DOCTORS WHO TREATED REAL COVID PATIENTS.
Dr. Didier Raoult, Dr Zelenko, Dr George Fareed and Dr Brian Tyson, Dr. Ben Marble and the doctors of “My Free Doctor”, Dr Darrell DeMello (who introduced early treatment, ER level treatment for the outpatient and long covid treatment to India), Dr Shankara Chetty with his outpatient "emergency room" 8th day protocol (teaching many Doctors and saving 10,000+ Africans and many others at a covid stage where they would be admitted to hospital then mis, dis and mal treated to either prolonged injury or death in most all US hospitals), Dr. Pierre Kory and Dr Paul Marik, Dr. Joseph Varon, Dr. Syed Haider and other doctors using the FLCCC protocols, Dr. Peter McCullough and Dr. Richard Urso, to name a few and numbers of other REAL DOCTORS who treated REAL COVID PATIENTS across the world. These Doctors treated 100’s of Thousands of high risk covid patients with near elimination of hospitalization and death with early treatment and with proper, asap, "ER" type treatment and these doctors demonstrated a great reduction of in hospital death with the best known practices.
These REAL DOCTORS TOLD THE TRUTHS, about covid treatments, with actually safe and effective, low cost generic drugs etc, TO THE POWERS THAT CHOOSE TO SUPPRESS AND SABOTAGE REAL TREATMENT FOR COVID. Powers that choose to push big pharma, not safe and not effective as used, high priced remdesivir etc and to push and compel a neither safe nor effective "vaccine" only path as a big pharma money maker and opportunity to force regulatory pre-approval status for the mRNA "platform" as a "vaccine" and genetic manipulation platform, not requiring further human testing. Which they accomplished with the mRNA bi-valent covid "vaccine" shots not tested in humans, based on the purportedly "safe and effective" mRNA platform use in the initial, forced mass covid "vaccinations".
EVERY ONE OF THESE DOCTORS DEMONSTRATED AN END TO THE “PANDEMIC”. 100% EASY for fda, cdc, nih, who, niaid and fauci et al. TO SEE AND KNOW the way to end the “pandemic”as THEY WERE INFORMED about working treatments, which they, et al, willfully, with treatment knowledge presented to them, CHOOSE NOT TO HEED while “they” SABOTAGED effective treatment protocols and REAL DOCTORS using these life saving protocols and thereby DEPRAVED-HEART MASS MURDERED MILLIONS. (DEPRAVED-HEART (indifference) MURDER see definition from "wickedpedia" below)
From "wickedpedia" – “In United States law, depraved-heart murder, also known as depraved-indifference murder, is a type of murder where an individual acts with a “depraved indifference” to human life and where such act results in a death, despite that individual not explicitly intending to kill. In a depraved-heart murder, defendants commit an act even though they know their act runs an unusually high risk of causing death or serious bodily harm to a person. If the risk of death or bodily harm is great enough, ignoring it demonstrates a “depraved indifference” to human life and the resulting death is considered to have been committed with malice aforethought.[1][2] In some states, depraved-heart killings constitute second-degree murder,[3] while in others, the act would be charged with “wanton murder,”[4][5] varying degrees of manslaughter,[6] or third-degree murder. If no death results, such an act would generally constitute reckless endangerment (sometimes known as “culpable negligence”) and possibly other crimes, such as assault.”
Common law background
It ["depraved heart" murder] is the form [of murder] that establishes that the wilful doing of a dangerous and reckless act (my note: sabotaging and suppressing REAL COVID TREATMENT and REAL DOCTORS TREATING COVID) with wanton indifference to the consequences and perils involved is just as blameworthy, and just as worthy of punishment, when the harmful result ensues as is the express intent to kill itself. This highly blameworthy state of mind is not one of mere negligence... It is not merely one even of gross criminal negligence... It involves rather the deliberate perpetration of a knowingly dangerous act with reckless and wanton unconcern and indifference as to whether anyone is harmed or not. The common law treats such a state of mind as just as blameworthy, just as anti-social and, therefore, just as truly murderous as the specific intents to kill and to harm.[7]
FEW DIE FROM COVID – MANY TORTURED AND MURDERED – BY FAILURE TO TREAT
Could the bar chart of outcomes by ethnicity be explained by Vitamin D? Whites>Asians>Hispanics>Blacks for Vit D production for a given level of sunlight exposure.